Guest article by Jennifer Coates, DVM
If your dog has recently been diagnosed with pancreatitis, it may seem like you have not been getting straightforward answers to your questions. The disease can be confusing, and not just for owners but for the veterinarians who treat it as well.
Pancreatitis can be no more serious than a mild “tummy ache,” or it can be a killer. Pancreatitis may be a one-time event with an obvious underlying cause, or it can occur over and over again despite the best treatment. Pancreatitis may have no long-lasting effect, or it may lead to severe complications down the road. And to top it all off, it is impossible to determine what a dog’s outcome might be at the disease’s onset. What initially looks like nothing serious can rapidly become a nightmare.
Let me go over the basics of this disease and try to clear up some of the confusion.
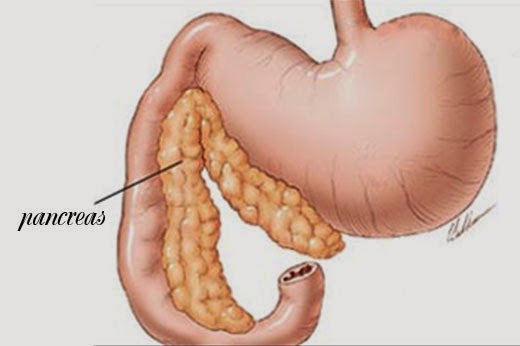
What is the Pancreas?
The pancreas is an abdominal organ that lies next to a portion of the small intestine. It has two major roles. It produces the hormone insulin that plays a critical role in regulating blood sugar levels, and it manufactures digestive enzymes that are pumped into the intestinal tract in response to a meal.
What is Pancreatitis?
The suffix “itis” means “inflammation of” in medical jargon. So pancreatitis simply means inflammation of the pancreas… but that is where the simplicity ends. The inflammation can develop for a number of reasons, one of the most well known is the ingestion of an especially fatty meal. Dogs that get into the trash or are fed lots of table scraps are at higher than average risk for developing pancreatitis. However, many dogs come down with the disease when there is no recent history of such an event. In these cases, an underlying problem like obesity, infection, metabolic disorders, trauma, breed predilection (e.g., schnauzers) or recent abdominal surgery might be to blame, but often a cause is ever found and we never know why the pancreas became inflamed in the first place.
But once the inflammation causes the pancreas to leak digestive enzymes onto its surface and into the abdomen, the situation starts to snowball. These enzymes are very irritating, essentially continuing their digestive function but now outside of the intestinal tract, and they incite even more inflammation. Permanent damage to the pancreas and surrounding organs is possible.
Diagnosis
Diagnosing pancreatitis is also not always easy. (What else did you expect?) A dog with a “typical” case of pancreatitis has a poor appetite, is lethargic, vomits, has diarrhea, has a fever, and his belly hurts. However, these symptoms are seen with many other diseases, and not every dog with pancreatitis looks like this, so diagnostic tests are necessary. Routine blood work may show an elevation in two pancreatic enzymes, amylase and lipase, but even if these levels are normal, pancreatitis is still possible. A more sensitive blood test called a cPLI is often run if the diagnosis is not clear. X-rays, an abdominal ultrasound, a urinalysis, a fecal examination, and even exploratory surgery may be necessary to diagnose some cases of pancreatitis and/or rule out other diseases that have similar symptoms.
Treatment
To stop the cycle of inflammation, the pancreas must stop secreting its digestive enzymes for a period of time. How is this done? By restricting what a pet eats. Dogs under treatment for pancreatitis are usually not offered any food or water by mouth until their symptoms are under control. To support the body and deal with dehydration, intravenous fluid therapy is usually necessary, although mildly affected dogs might be able to get away with fluids injected under their skin. If a dog is not beginning to recover after several days, he may need to be fed via a tube that is surgically inserted into his intestinal tract below where the pancreas empties or perhaps receive nutrition directly into his bloodstream.
Nausea and pain-relieving medications are a very important part of pancreatitis treatment. Antibiotics are often used in case a bacterial infection is involved and to prevent the formation of pancreatic abscesses. If an abscess develops, surgery will be required to drain it. Plasma transfusions can be a life-saver in severe cases of pancreatitis.
Once a dog is able to eat and drink again, he will usually be offered small, frequent meals of a low-fat, easily digested diet and will be closely monitored for relapses. Low fat diets may be prescribed in the long term in an attempt to prevent future flare-ups. If the pancreas has been severely damaged, it may not be able to perform its normal functions of producing insulin and digestive enzymes. Diabetes mellitus or pancreatic insufficiency can result, and if these or other complications develop, additional treatment will be necessary.
Many dogs with pancreatitis recover uneventfully and go on to live normal lives, but these are the lucky ones. Unfortunately for some, pancreatitis can be a life-altering, or ending, disease.
***
Jennifer Coates, DVM graduated with honors from the Virginia-Maryland Regional College of Veterinary Medicine in 1999. In the years since, she has practiced veterinary medicine in Virginia, Wyoming, and Colorado. She is the author of several books about veterinary medicine and animal care, including the Dictionary of Veterinary Terms: Vet-speak Deciphered for the Non-veterinarian. Jennifer also writes short stories that focus on the strength and importance of the human-animal bond and freelance articles relating to a variety of animal care and veterinary topics. Dr. Coates lives in Fort Collins, Colorado with her husband, daughter, and pets.
Related stories:
The House Is On Fire! Bridget's Pancreatitis
If your dog has recently been diagnosed with pancreatitis, it may seem like you have not been getting straightforward answers to your questions. The disease can be confusing, and not just for owners but for the veterinarians who treat it as well.
Pancreatitis can be no more serious than a mild “tummy ache,” or it can be a killer. Pancreatitis may be a one-time event with an obvious underlying cause, or it can occur over and over again despite the best treatment. Pancreatitis may have no long-lasting effect, or it may lead to severe complications down the road. And to top it all off, it is impossible to determine what a dog’s outcome might be at the disease’s onset. What initially looks like nothing serious can rapidly become a nightmare.
Let me go over the basics of this disease and try to clear up some of the confusion.
What is the Pancreas?
The pancreas is an abdominal organ that lies next to a portion of the small intestine. It has two major roles. It produces the hormone insulin that plays a critical role in regulating blood sugar levels, and it manufactures digestive enzymes that are pumped into the intestinal tract in response to a meal.
What is Pancreatitis?
The suffix “itis” means “inflammation of” in medical jargon. So pancreatitis simply means inflammation of the pancreas… but that is where the simplicity ends. The inflammation can develop for a number of reasons, one of the most well known is the ingestion of an especially fatty meal. Dogs that get into the trash or are fed lots of table scraps are at higher than average risk for developing pancreatitis. However, many dogs come down with the disease when there is no recent history of such an event. In these cases, an underlying problem like obesity, infection, metabolic disorders, trauma, breed predilection (e.g., schnauzers) or recent abdominal surgery might be to blame, but often a cause is ever found and we never know why the pancreas became inflamed in the first place.
But once the inflammation causes the pancreas to leak digestive enzymes onto its surface and into the abdomen, the situation starts to snowball. These enzymes are very irritating, essentially continuing their digestive function but now outside of the intestinal tract, and they incite even more inflammation. Permanent damage to the pancreas and surrounding organs is possible.
Diagnosis
Diagnosing pancreatitis is also not always easy. (What else did you expect?) A dog with a “typical” case of pancreatitis has a poor appetite, is lethargic, vomits, has diarrhea, has a fever, and his belly hurts. However, these symptoms are seen with many other diseases, and not every dog with pancreatitis looks like this, so diagnostic tests are necessary. Routine blood work may show an elevation in two pancreatic enzymes, amylase and lipase, but even if these levels are normal, pancreatitis is still possible. A more sensitive blood test called a cPLI is often run if the diagnosis is not clear. X-rays, an abdominal ultrasound, a urinalysis, a fecal examination, and even exploratory surgery may be necessary to diagnose some cases of pancreatitis and/or rule out other diseases that have similar symptoms.
Treatment
To stop the cycle of inflammation, the pancreas must stop secreting its digestive enzymes for a period of time. How is this done? By restricting what a pet eats. Dogs under treatment for pancreatitis are usually not offered any food or water by mouth until their symptoms are under control. To support the body and deal with dehydration, intravenous fluid therapy is usually necessary, although mildly affected dogs might be able to get away with fluids injected under their skin. If a dog is not beginning to recover after several days, he may need to be fed via a tube that is surgically inserted into his intestinal tract below where the pancreas empties or perhaps receive nutrition directly into his bloodstream.
Nausea and pain-relieving medications are a very important part of pancreatitis treatment. Antibiotics are often used in case a bacterial infection is involved and to prevent the formation of pancreatic abscesses. If an abscess develops, surgery will be required to drain it. Plasma transfusions can be a life-saver in severe cases of pancreatitis.
Once a dog is able to eat and drink again, he will usually be offered small, frequent meals of a low-fat, easily digested diet and will be closely monitored for relapses. Low fat diets may be prescribed in the long term in an attempt to prevent future flare-ups. If the pancreas has been severely damaged, it may not be able to perform its normal functions of producing insulin and digestive enzymes. Diabetes mellitus or pancreatic insufficiency can result, and if these or other complications develop, additional treatment will be necessary.
Many dogs with pancreatitis recover uneventfully and go on to live normal lives, but these are the lucky ones. Unfortunately for some, pancreatitis can be a life-altering, or ending, disease.
***
Jennifer Coates, DVM graduated with honors from the Virginia-Maryland Regional College of Veterinary Medicine in 1999. In the years since, she has practiced veterinary medicine in Virginia, Wyoming, and Colorado. She is the author of several books about veterinary medicine and animal care, including the Dictionary of Veterinary Terms: Vet-speak Deciphered for the Non-veterinarian. Jennifer also writes short stories that focus on the strength and importance of the human-animal bond and freelance articles relating to a variety of animal care and veterinary topics. Dr. Coates lives in Fort Collins, Colorado with her husband, daughter, and pets.
Related stories:
The House Is On Fire! Bridget's Pancreatitis

Comments
Post a Comment